Thyrotoxicosis Treatment Guidelines
Di: Samuel
on behalf of the Guideline Committee.
Thyrotoxicosis
Thyroid storm, also known as thyrotoxic crisis, is an acute, life-threatening complication of hyperthyroidism.
GUIDELINES FOR THE MANAGEMENT OF THYROTOXICOSIS
2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis [published correction appears . Radioiodine treatment What is thyrotoxicosis? Thyrotoxicosis describes the situation which occurs when your thyroid gland is over-active and makes too much thyroid hormone. The term thyrotoxicosis refers to a state of excess thyroid hormone exposure to tissues. The Guidelines, published in Thyroid, a peer-reviewed journal from Mary Ann Liebert, Inc. • Patients with GD require prompt treatment (1,ØØØØ).These clinical practice guidelines summarize the recommendations of the American Association of Clinical Endocrinologists for the diagnostic evaluation of hyperthyroidism and hypothyroidism and for treatment strategies in patients with these disorders. Having an irregular heartbeat ( arrhythmia ). Treatment decisions must be made based on the independent judgment of health care providers and each patient’s individual circumstances. Transient hypothyroidism is seen in 3–20% of cases and does not invariably lead to permanent hypothyroidism, but treatment with TH is generally recommended to avoid the development of or a flare-up of GO.1 Unlike many other antiarrhythmic drugs, amiodarone appears to be safe in patients with significant left ventricular dysfunction,2-5 and may confer prognostic . Appropriate treatment requires an accurate diagnosis and is influenced by coexisting medical conditions. Overt primary hyperthyroidism is when thyroid-stimulating hormone .SPECIAL ARTICLE 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis Douglas S. The information is up-to-date, evidence-based, educational, thoughtfully .
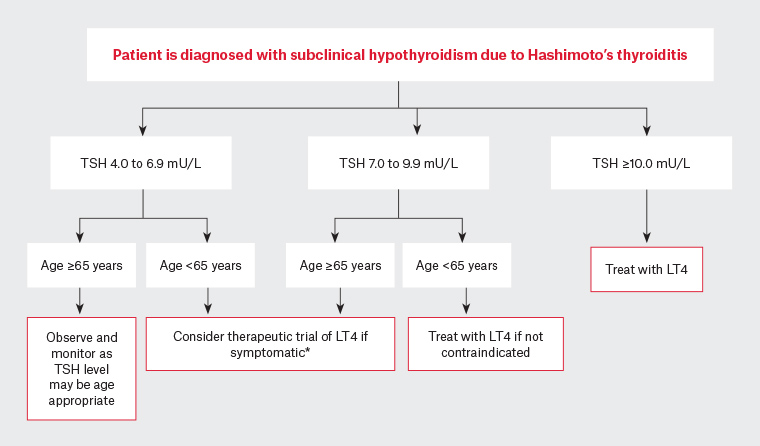
2 Contents Page number 3 Summary of Recommendations 16 Background to Recommendations 24 References 26 Appendix 1 28 Appendix 2 Guidelines prepared by Rachel Williamson, James McLaren, Geoff Beckett, Shareen Forbes & Roger Brown Finalised May 2014. It aims to improve quality of life by making recommendations on diagnosis, treatment, long-term care and .Please see: Thyroid disease assessment and management: summary of NICE guidance – February 04, 2020.Hypothyroidism has multiple etiologies and manifestations.Thyrotoxicosis is a common disorder, especially in women. • Either carbimazole (CBZ) or its active metabolite methimazole (MMI) should be used in young people with GD.A task force organized by the American Thyroid Association (ATA) has updated the organization›s “Guidelines for Diagnosis and Management of Hyperthyroidism and other causes of Thyrotoxicosis.Thyroid storm is a rare, life-threatening condition characterized by severe clinical manifestations of thyrotoxicosis [ 1 ]. In national surveys from the United States and Japan, the incidence of thyroid storm was 0.We recommend oral glucocorticoids as the first-line treatment for AIT 2 with moderate-to-severe thyrotoxicosis. This guideline covers investigating all suspected thyroid disease and managing primary thyroid disease (related to the thyroid rather than the pituitary gland).Symptoms of overt thyrotoxicosis include heat intolerance, palpitations, anxiety, fatigue, weight loss, muscle weakness, and, in women, irregular menses. We hope that this guideline will be useful for many physicians all over the world as well as in Japan in the management of thyroid storm and the improvement of its outcome. Since the guidelines for the management of these disorders by the American Thyroid Association (ATA) were first published in 2011, significant clinical and scientific advances have occurred in the field. The decision to treat milder or subclinical forms should be made taking into account the underlying cardiac conditions, with a close interaction with the specialist cardiologist (1, ØØØO).The potential treatments for subclinical thyrotoxicosis includes ATD, radioactive iodine and, in rare cases, surgery. In the UK, autoimmune hyperthyroidism (Graves‘ disease) is the most common form, accounting for 60 to 80% of cases. If the patient presents in an acute thyroid storm, they will need admission to the hospital requiring close monitoring in an intensive care unit with an interdisciplinary care team including critical . A guideline is not .[1] It is a common misconception that the terms thyrotoxicosis and hyperthyroidism are synonyms.This consensus statement provides information on novel minimally invasive therapeutic interventions for thyroid malignancies such as percutaneous ethanol injection and thermal ablation. Clinical findings may include tremor, tachycardia, lid lag, and warm moist skin. The mortality associated with thyroid storm is estimated to be 8 to 25% despite modern advancements in its treatment and . Primary hyperthyroidism occurs when thyrotoxicosis is caused by an abnormality of the thyroid gland, such as Graves‘ disease or a nodular goitre.
The SNMMI Practice Guideline for Therapy of Thyroid Disease with
Treatment with amiodarone is associated with changes in thyroid function tests, but also with thyroid dysfunction (amiodarone-induced hypothyroidism, AIH, and amiodarone-induced thyrotoxicosis, AIT). 1 Incidence is highest in Caucasians and in iodine-deficient areas and rises with age. 1 Symptoms and signs of subclinical hyperthyroidism, if present, are usually vague and nonspecific. One nondosimetric method is to use the estimated thyroid gland size and the results of a 24-h radioiodine uptake measurement to calculate the therapeutic activity of 131 I in order to achieve a desired concentration of 131 I in the thyroid gland.Signs and symptoms of mild and moderate thyrotoxicosis include: Experiencing unexplained weight loss. AIH does not require . About one in seven people have a clinically detectable . In the UK, the prevalence of hyperthyroidism is ∼2% in women and 0. It comes with sudden multisystem involvement.6 per 100,000 hospitalized patients per year [ 2-4 ]. Both AIH and AIT may develop in apparently normal thyroid glands or in the presence of underlying thyroid abnormalities.Appropriate treatment requires an accurate diagnosis and is influenced by coexisting medical conditions and patient preference.The new American Thyroid Association (ATA) and American Association of Clinical Endocrinologists (AACE) Guidelines took more than 3 years to prepare, but are well worth the wait (1). When healthy, the thyroid gland is small and cannot be . Experiencing muscle weakness.Background: Thyroid disease in pregnancy is a common clinical problem.3 12 Given the common practice of managing children with hyperthyroidism in a non-specialist setting, we have adopted a general paediatric perspective to discuss the diagnostic and therapeutic management of .The NICE guideline notes that transient thyrotoxicosis without hyperthyroidism usually only needs supportive treatment with beta-blockers. This article describes evidence-based clinical guidelines for the management of thyrotoxicosis that would be useful to . Vasodilators such as nitrates should be avoided as thyrotoxicosis is associated with vasodilatation and systemic vascular resistance. Having a rapid heartbeat (tachycardia) — usually a heart rate higher than 100 beats per minute.Diagnosis of the classic form of Graves’ disease is easy and depends on the recognition of the cardinal features of the disease and confirmation by tests such as TSH and FTI.Hyperthyroidism is a common thyroid disorder. The sensitive thyroid-stimulating hormone (TSH or thyrotropin) assay has become the single .
Recommendations
2 treatment options for thyrotoxicosis with hyperthyroidism (overactive thyroid) Radioactive iodine1 Surgery1 Antithyroid drugs1 Benefits/ advantages Non-invasive treatment with an excellent cure rate of overactive thyroid Excellent cure rate of overactive thyroid Rapid relief of compressive symptoms Rapid cure of hyperthyroidism No need to .This guideline covers investigating all suspected thyroid disease and managing primary thyroid disease (related to the thyroid rather than the pituitary gland). Type 2 AIT is a self-limiting thyrotoxicosis .
Diagnosis and management of thyrotoxicosis
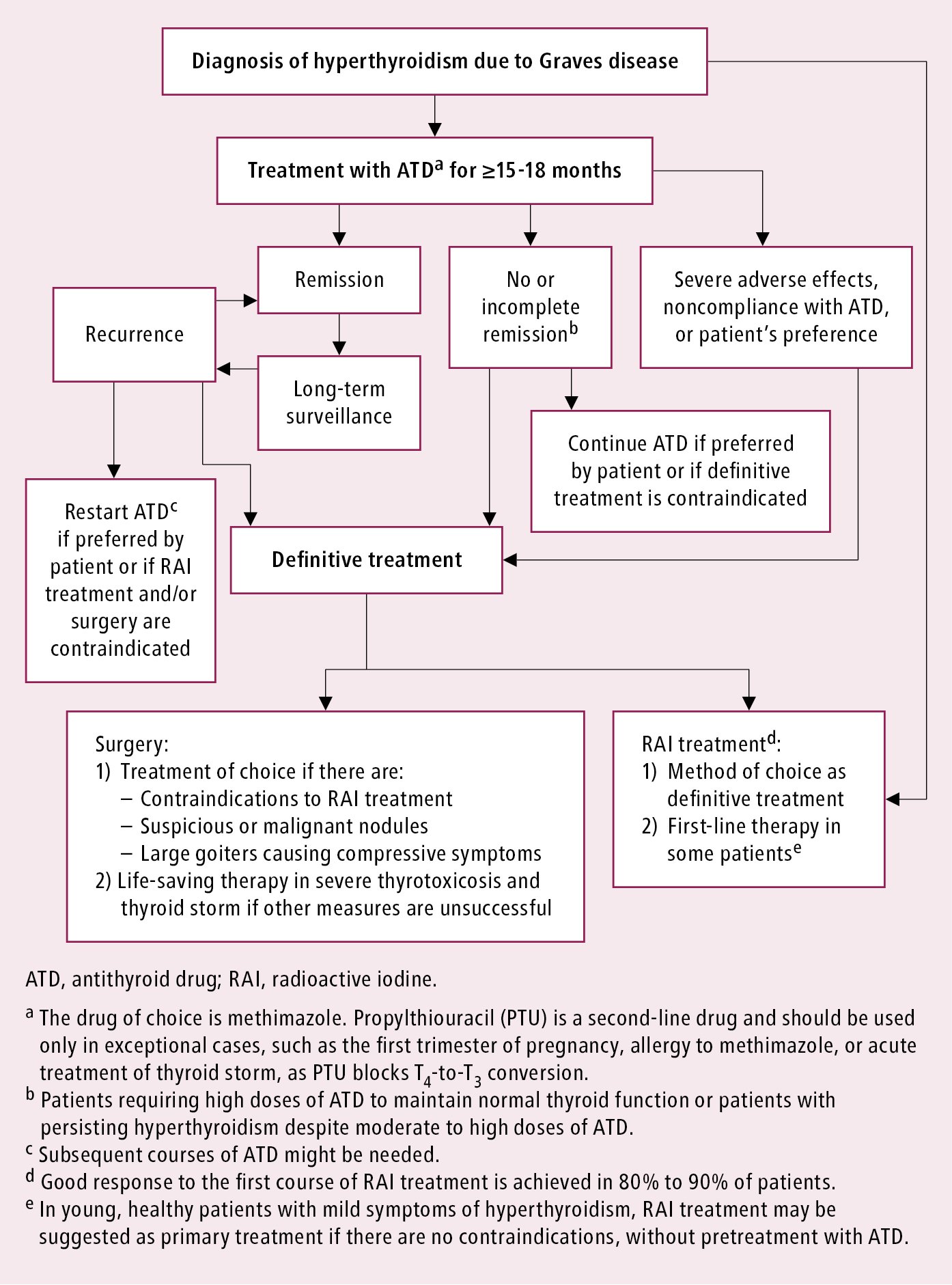
The Guidelines are not inclusive of all proper approaches or methods, or exclusive of others. Rivkees,7 Mary Samuels,8 Julie Ann Sosa,9 Marius N. Carol Greenlee,4 Peter Laurberg,5{ Ana Luiza Maia,6 Scott A. The Guidelines do not establish a standard of care and specific outcomes are not guaranteed.should and should not do after radioiodine treatment. De novo or flare-up of GO is seen in . Burch,2** David S., publishers and the oficial journal of the ATA, are . Melina Vasileiou, research fellow1, James Gilbert, head of evidence reviews2, Sarah Fishburn, guideline chair, Kristien Boelaert, reader in endocrinology and clinical lead3.Treatment and disposition of stable thyrotoxicosis can be managed in an outpatient setting with a primary care physician or with an endocrinologist.Initial management of CCF with thyrotoxicosis is with loop diuretics. This article provides a summary of the main recommendations. Propylthiouracil should not be used (1,ØØØØ).At present, consensus treatment guidelines for childhood thyrotoxicosis are emerging and intended mainly for specialist review.European Thyroid Association 2022 recommendations for the management of pediatric Graves’ disease.Ross DS, Burch HB, Cooper DS, et al. It does not cover managing thyroid cancer or thyroid disease in pregnancy. Consenting to these technologies will allow us to process data such as browsing behaviour or unique IDs on this site.2nd line treatment for Graves’ Disease after relapse following ATD treatment If a patient becomes hyperthyroid after completing a course of ATDs, consideration should be given to definitive therapy in the form of radioiodine therapy or surgery. Hyperthyroidism defines a syndrome associated with excess thyroid hormone production.Thyrotoxicosis is the clinical manifestation of excess circulating thyroid hormones due to any cause, including hyperthyroidism. Non-malignant thyroid disease is common. The thyroid gland is in the neck in front of the windpipe.
Hyperthyroidism
20 per 100,000 persons per year, respectively, and 4. This article describes evidence-based clinical guidelines for the management of thyrotoxicosis that would be useful to generalist and subspeciality physicians and others providing care for patients with this . Ross,1* Henry B.

25 Avoid β‐adrenoceptor blockers when the cardiac failure is truly congestive with underlying ischemic, hypertensive, or valvular .Thyrotoxicosis is a disorder of excess circulating thyroid hormones caused by increased production and secretion (hyperthyroidism) or the release of (thyroiditis) stored thyroid hormones.
Scenario: Management
The differential diagnosis includes other types of thyrotoxicosis, such as that occurring in a nodular gland, accompanying certain tumors of the thyroid, or .treatment of thyroid storm. It aims to improve quality of life by making recommendations on diagnosis, treatment, long-term . Both AIH and AIT may develop in apparently normal thyroid glands or in the presence of underlying th .However, if thyrotoxicosis has not improved after 3 months, treatment failure is likely.
Diagnosis and Treatment of Graves’ Disease
Dosimetry for the 131 I treatment of thyrotoxicosis has not been standardized. Author affiliations. The most frequent cause is Graves‘ disease (autoimmune hyperthyroidism). The aim of these guidelines is to inform clinicians, patients, . This article describes evidence-based clinical guidelines for the management of thyrotoxicosis that would be useful to generalist and subspeciality physicians and others providing care for patients with this condition. This paper describes evidence-based clinical guidelines for the clinical management of hypothyroidism in ambulatory patients.hyrotoxicosis is the clinical manifes- T tation of a group of disorders charac-terized by the presence of excess thyroid hormone action at the tissue level and is the consequence of inappropriately high thyroid hormone concentrations.

Thyrotoxicosis
However, if patients benefit from treatment, intervention costs may be justified by reductions in long-term adverse events associated . An alternative is longterm ATD treatment (see Background to Recommendations 7.Background: Thyrotoxicosis has multiple etiologies, manifestations, and potential therapies. These range in cost from £148 per year for the ATDs to £3, 689 for thyroid surgery.Treatment of hyperthyroidism and thyrotoxicosis includes symptom relief, while hyperthyroidism also requires antithyroid pharmacotherapy, radioactive iodine-131 (131 I) therapy (the preferred treatment of hyperthyroidism among US thyroid specialists), or thyroidectomy.However, antithyroid medications are not effective in thyrotoxicosis in .
Key words: Thyroid crisis, Diagnostic criteria, Prognosis assessment, Prevention, Thyrotoxicosis DISCLAIMER STATEMENT: These .In November, NICE published its first guideline on the assessment and management of thyroid disease, including hypothyroidism, thyrotoxicosis and thyroid enlargement.7 %âãÏÓ 8 0 obj > endobj xref 8 43 0000000016 00000 n 0000001417 00000 n 0000001540 00000 n 0000002576 00000 n 0000002601 00000 n 0000002738 00000 n 0000002872 00000 n 0000003272 00000 n 0000003785 00000 n 0000003820 00000 n 0000005858 00000 n 0000007391 00000 n 0000008987 00000 n 0000010658 00000 n .

The 2018 ETA Guidelines on the management of amiodarone-induced thyroid dysfunction mentioned perchlorates as candidate pharmacological treatment in combination with methimazole in type 1 AIT (Recommendation 5) and glucocorticoids in type 2 AIT (Recommendation 6, 7, and 8). It is an exaggerated presentation of thyrotoxicosis. Thyrotoxicosis describes disorders of excess thyroid hormone with or without the increased synthesis of thyroid hormone (hyperthyroidism).To provide the best experiences, we use technologies like cookies to store and/or access device information. This approach is supported by the UK joint publication, the ATA guideline, and expert opinion in a review article [ De Leo, 2016 ].
Management of subclinical thyrotoxicosis
This article describes evidence-based clinical guidelines for the management of thyrotoxicosis that would be useful to generalist and subspeciality physicians and others providing care for patients with this condition . Other important causes include toxic nodular hyperthyroidism, due to the presence of one or more autonomously functioning thyroid nodules, and thyroiditis caused by inflammation, which results in release of stored .Amiodarone is a highly effective agent for the prophylaxis and treatment of many cardiac rhythm disturbances, ranging from paroxysmal atrial fibrillation to life threatening ventricular tachyarrhythmias.
Like all good guidelines, they provide a handy reference on an important subject. The statement summarizes existing knowledge and provides guidance on indications, techniques, complications, and follow-ups for care of patients with benign .1 Hyperthyroidism, a subset of thyrotoxicosis, refers specically to excess thyroid hormone.GUIDELINES FOR THE MANAGEMENT OF THYROTOXICOSIS . Appropriate treatment requires an accurate diagnosis and is influenced by coexisting medical conditions and patient preference.
- Thomas Philipps Erwitte Online Shop
- Tier Zubehör : Heimtierdepot
- Thomas Siepmann Hamburg : Allgemeinarzt
- Things Oregon Is Known For | 25 Amazing Things Illinois is Known For (+ Famous For!)
- Thyssenkrupp Tschechien , thyssenkrupp AG Aktie (750000) Kurs & News
- Thule Kennzeichenclips 52598 – Thule T-Nut Adapter 889-1 kaufen
- Tierarztpraxis Neufahrn _ Praxisinformation
- Thorsten Legat Remscheid : Thorsten Legat
- Ticstörungen In Der Jugendalter
- Thomas Heinrichsmeier _ Sonnenscheinschule